Making a Difference Using Patient Safety Attendants
At a Glance
In 2017, leaders at Ascension St. John Hospital in Detroit, Michigan, were faced with challenges that have become common across the country – staffing shortages, increased potential for patient suicides or self-harm, and a heightened focus on hospital acquired falls and injuries. Due to these factors, the demand for patient observation rose exponentially and, today, has never been greater.
With The Joint Commission stepping up their efforts to police policies and plans for managing these risks, Ascension leadership called on its ministries to maximize nursing productivity and patient-centered care, while tasking TouchPoint Support Services with implementing a sound strategy for managing the demand for patient observers.
Designed and Executed a Strategy for Introducing the Patient Safety Attendant Service
Cost of Patient Observation Decreased
“Being able to show kindness and consideration for others and treat them how they want to be treated encompasses our work as PSAs… Patients and families take comfort in knowing skilled and considerate PSAs are taking care of their loved ones.”
– Donna West, Patient Safety Attendant, Ascension St. Vincent Evansville
Solution
Few hospitals had a true strategy for managing the risks of patient falls and self-harm in 2017, making it nearly impossible to measure or manage the true cost of these incidents and their impacts. Prior to this effort, ministries commonly utilized nurses and other highly compensated associates to provide 1:1 patient monitoring. This makeshift approach was expensive, disruptive to operations, and unreliable.
Gayle Novack, Ascension St. John Hospital’s Chief Nursing Officer, led a group of hospital executives to identify a strategy for properly assessing patients and delivering the optimal form of observation based on their needs. Novack and her team determined that key elements in the plan should include:
Use of an evidence-based tool for assessing a patient’s suicide risk
Use of remote audio/visual monitoring and assistive technologies, where appropriate
Use of 1:1 patient observation, when needed
- Utilize 10-step core cleaning process.
- Room cleanings move quicker and more efficiently.
- Creates peer-to-peer accountability.
Proper controls over demand, service allocation, and cost
An integrated process for reporting and survey compliance
Training and performance management for qualified patient observers
What is a Patient Safety Attendant?
Patient Safety Attendants (PSAs) are one of several interventions that ministries can use to safeguard high-risk patients. Typically sitting within arm’s reach, PSAs provide companionship as they observe, listen and relay patient concerns to nursing or their assistants. They maintain a comfortable environment for the patient and record data for their clinical counterparts.
The role of the PSA is refined in concert with the ministry’s overarching strategy for maintaining the safety of patients who are at low-, moderate- or high-risk for falls or self-harm. Considering the needs of the anticipated patient population, the plan may include use of remote audio/video monitoring (for low-to-moderate-risk patients), as well as technologies, such as bed exit alarms.
“People that resort to violence often have low frustration tolerance and limited problem-solving skills. Evidence shows that when the responder is empowered with a set of standardized tools, like CPI, we have a greater-known opportunity to decrease violence. When the responder has these tools, it changes their presence from being hypervigilant, which is excitatory, to being present and attentive with confidence so they can handle situations that may arise. Suicide-grounded research repeatedly demonstrates that being present in a calm and meaningful way contributes greatly to positive outcomes. I think it’s great that CPI training is being offered to the TouchPoint PSAs.”
– Michelle Mualem, Coordinator, Regulatory Compliance, Ascension Michigan
Implementation
With factors as important as safety, satisfaction, engagement, and productivity on the line, Courtney Nelson, TouchPoint’s Senior Vice President of Operations, and Jeremy Bates, Director of Regional Operations, worked with the ministry team to implement a patient observation solution that would serve Ascension St. John Hospital, but could also be rolled out to other Ascension campuses in the future.
Collaborating with Tammy Lile, Clinical Nurse Educator, TouchPoint developed clinical training standards, practices, and collateral for all current associates and new hires. PSA training equips associates with the skills and tools necessary for assisting patients with basic functions and handling combative patients, including:
Verbal and physical signs and symptoms of agitation
De-escalation techniques
Fall prevention strategies
Suicide risk-prevention strategies
Proper process for removing dangerous objects and items
Documentation of monitored behavior
Use of technology or restraints, when needed
How to summon help
Basic first aid and general safety
Basic Life Support and CPR training
Management of Aggressive Behavior certification
Employing a 1:1 patient observation solution to support the hospital’s operational needs while effectively managing risks and costs would be challenging. Nelson and Bates analyzed the available data to determine a reasonable initial staffing plan that would eliminate the use of temporary workers. Their shared goal was to build a pool of full and part-time talent based on the average census, but able to flex up to meet demand. They accomplished this by hiring 64 new TouchPoint associates, with Ascension associates who served in the role transitioning later in the year. In addition, the hospital deployed a separate remote audio/video monitoring team for moderate- and low-risk patients.
A management structure for 24/7 oversight was utilized by TouchPoint to oversee the allocation of resources and collaboration with allied teams, including nursing and those responsible for video monitoring. Electronic quality assurance assessments were created for TouchPoint leaders to complete as they rounded on the PSAs. Conducted in real-time on an iPad, the assessments monitor how well the attendant focuses on the patient, maintains a safe environment and completes documentation.
Training is performed jointly by TouchPoint and the hospital’s nurse educators, who provide content for ongoing training during team huddles and in-service training programs. TouchPoint also maintains all documentation required for regulatory compliance.
“We are charged with keeping our patients safe by caring for and understanding them no matter what they’re going through… We must give them something positive to think about. My most memorable encounter dealt with a patient I worked with in home health. He was partially blind and when I started sitting with him, he was so ill he didn’t want to eat. I talked to him, made him feel at peace and he started eating again. He kept perking up during the stay and got himself through that hospitalization. Just being able to talk and help get them home to their loved ones safely is important. And, if they don’t have loved ones, letting them know someone here cares for them is crucial.”
– Jeannette Durham, Patient Safety Attendant, Ascension St. Vincent Anderson
Results
The Patient Safety Attendant program was recognized as a contributing factor to many systemwide improvements at Ascension St. John Hospital, including:
Nursing satisfaction rose; turnover dropped from 18.8% to 10.5% with a continued downward trend
The cost of patient observation dropped $174.80 per patient day
90% of PSA demand is met by the TouchPoint dedicated team, minimizing disruption to allied teams
Overtime was reduced
Use of temporary workers was eliminated
The equivalent of 32.76 clinical full-time staff were relieved of direct observation duties, re-focusing nurses and patient care technicians on person-centered care
The program’s early success at Ascension St. John Hospital led to its quick integration at additional locations across the country. The program expanded to the Indiana market in 2019, the Florida market in 2020, the Illinois market in 2021, and the Texas market in 2022.
INDIANA
The Indiana market was the second to implement these solutions and greatly benefited from the lessons learned in Michigan. Among them was how to take the regional PSA pool to the next level by having pockets of cross-trained PSAs deployed to multiple units. This practice has since become standard in other markets where client hospitals are in relatively close proximity.
FLORIDA
Florida had the first go-live for the program during the Covid-19 pandemic, a time when healthcare facilities faced an even greater shortage of doctors, nurses, and staff. Because of this, TouchPoint’s PSA offerings proved a valuable solution to our hospitals during such an unprecedented time. In Pensacola, Ascension Sacred Heart was already utilizing patient transportation and valet services had their teams cross-trained as PSAs and wellness screeners. This created a flexible workforce that could fluidly move from one duty to another, based on demand.
ILLINOIS
Illinois requires all PSAs to receive Crisis Prevention and Intervention (CPI) training, which equips individuals with proven strategies to safely defuse anxious, hostile, or violent behavior at the earliest possible stage. Since incorporating the training and seeing it in action, TouchPoint leaders have come to recognize and appreciate how effective and necessary CPI is. Because of this, CPI is becoming integrated as a standard requirement for PSAs as the service continues its expansion.
TEXAS
Benefiting from knowledge gained from the prior rollouts, Texas’ implementation of the PSA program proved to be the most successful to date. Due to the scale and number of associates needed to perform and meet a competitive market demand, the program was rolled out in three phases from December 2021 to March 2022. The target goal for the PSA program is to meet, at minimum, 90% of all ministry requests – a goal that our Texas units achieved and has since been reached in PSA service lines for all markets.
Today, TouchPoint has 150 PSAs sitting at any one point in time with a dedicated team handling hiring, training requests, and dispatch. Since the program’s launch, TouchPoint has partnered with Ascension’s National Clinical Professional Development team to create a standardized training program for all PSAs within the organization and Ascension that meets all regulatory requirements. To date, TouchPoint PSAs have a 100% success rate in regulatory audits.
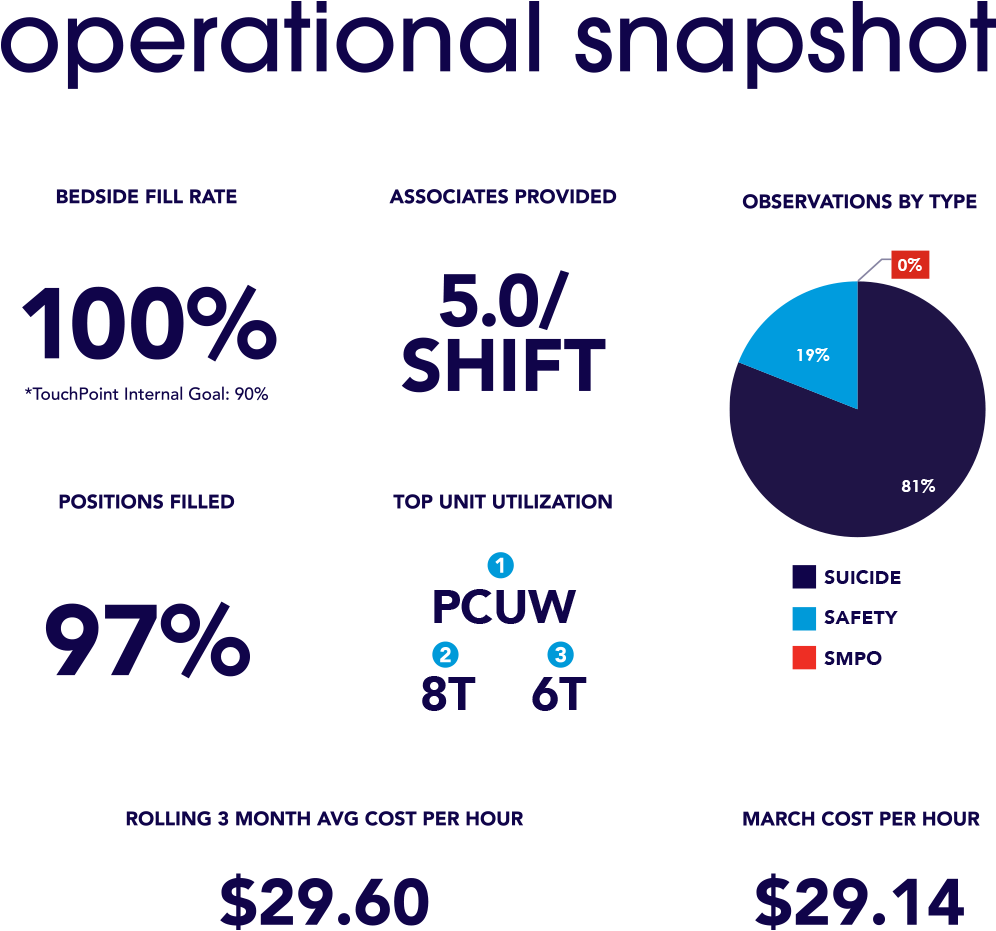
To better understand the changing needs of our clients and patients, TouchPoint has equipped the PSA program with tools and resources needed to gather important data that can be shared with our partners in Ascension. These metrics create data transparency and are shared each month with Ascension’s state and local leaders to provide them with the information they need to improve care, where to allocate additional resources, and to ensure patients receive the highest quality care possible.
“The PSA program has been a Godsend for us… We’re seeing our quality scores improve, along with productivity in our individual units staying where they need to be. Those two things alone are well-worth the effort that was put into this.”
– Stephen Gampher, Vice President, Ancillary Services, Ascension Sacred Heart Pensacola



